Evidence-Based, Trauma-Informed Psychiatric Support for PTSD, C-PTSD, and Trauma-Related Symptoms
Trauma changes how the brain processes emotion, memory, safety, and threat — but with the right support, the brain can heal.
Trauma-focused psychiatric care helps reduce the intensity of trauma symptoms, regulate the nervous system, improve sleep, and create the stability needed for deeper therapeutic work.
At Arizona Mental Wellness, our trauma-focused psychiatry approach is built on safety, compassion, and collaboration.
We understand that trauma shows up in emotional, physical, cognitive, and relational ways — and that healing requires individualized, gentle care.

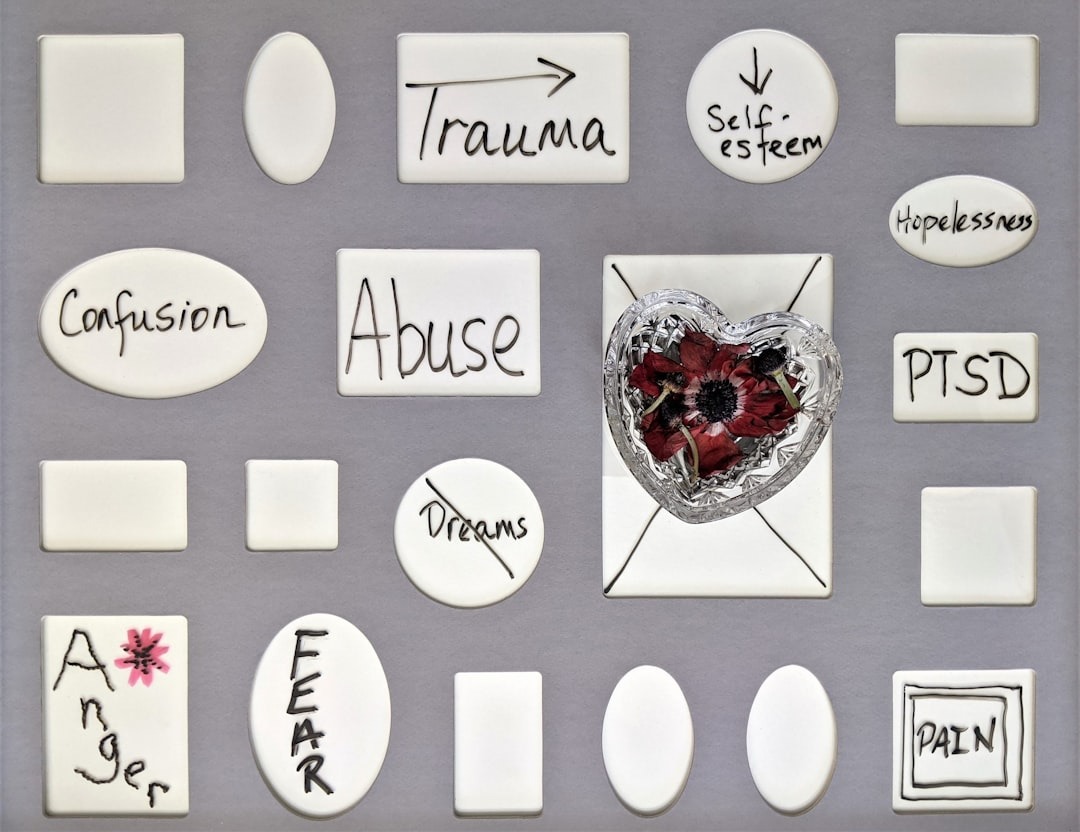
How Trauma Impacts the Brain & Nervous System
Trauma can leave lasting effects on:.
Emotional Regulation
- Heightened reactivity
- Intense irritability
- Difficulty calming down
- Emotional numbness
Cognitive Function
- Difficulty concentrating
- Overthinking
- Memory disruptions
- Negative self-beliefs
Physical Responses
- Hypervigilance
- Strong startle response
- Sleep disruption
- Exhaustion or fatigue
Trauma reactions are survival responses — not character flaws. Psychiatry helps calm the nervous system so healing can happen.
Conditions We Treat in Trauma-Focused Psychiatry
We provide specialized psychiatric support for:
Psychiatric Evaluations
- PTSD
- Complex Trauma (C-PTSD)
- Trauma-related anxiety or depression
- Panic symptoms
- Emotional dysregulation
- Mild to moderate dissociation
- Nightmares & Sleep Disturbance
- Trauma connected with ADHD or Autism
Medication Management
Careful medication planning to stabilize symptoms and support your recovery journey.
Our approach is slow, steady, collaborative, and never rushed.
Our Approach
Discover how our trauma-focused psychiatry guides you through healing with clear, compassionate steps tailored to your recovery journey.
What a Trauma-Focused Psychiatric Evaluation Includes
We prioritize emotional safety and stabilization at every step.
A trauma-focused evaluation may explore:
- Current symptoms (without needing to describe traumatic events)
- Triggers and stress responses
- Sleep and nightmare patterns
- Mood, irritability, and anxiety
- Nervous system activation
- Co-occurring diagnoses (ADHD, depression, anxiety, bipolar)
- Medical history and previous treatments
- Your coping skills and safety supports
- What helps you feel grounded
- Your goals and comfort level
You control the pace.
You never have to share details you don’t want to.
Trauma-Focused Psychiatry for Neurodivergent Clients
Many autistic and ADHD adults experience lifelong trauma from:
- Masking
- Chronic invalidation
- Sensory overwhelm
- Social challenges
- Rejection sensitivity (RSD)
- Identity trauma
Our neurodiversity-affirming model includes:
- Sensory-safe treatment planning
- Emotion regulation tools
- Gentle medication titration
- Respect for communication style
- Shame-free interpretations
- Executive functioning support
Your brain deserves care that understands it.
Psychiatry + Trauma Therapy = Best Outcomes
Psychiatry stabilizes the body.
Therapy heals the wounds.
Psychiatry supports:
- Sleep
- Anxiety
- Mood stability
- Emotional regulation
- Hyperarousal
Therapy supports:
- Trauma processing
- Attachment healing
- Coping skills
- Narrative integration
- Identity and relational safety
When to Seek Trauma-Focused Psychiatric Care
You may benefit from psychiatric support if you experience:
- Nightmares or severe sleep problems
- Hypervigilance
- Panic attacks
- Emotional overwhelm/shutdown
- Difficulty functioning
- Intrusive thoughts or memories
- Flashback-like episodes
- Anger or irritability
- Deep shame or negative beliefs
- Worsening anxiety or depression
- Feeling “stuck” despite therapy
You deserve relief, safety, and support.
You Can Heal — And You Don’t Have to Do It Alone
Trauma-focused psychiatric care helps you feel safer, more grounded, and more in control.
Healing is not linear — but it is absolutely possible.
👉 Schedule a Trauma-Focused Psychiatry Appointment
📞 (XXX) XXX-XXXX
📧 info@arizonamentalwellness.com
Your healing matters — and your safety comes first.
A: Trauma-focused psychiatry integrates trauma-informed principles into every part of care. This includes evaluating symptoms with sensitivity, understanding how trauma affects the brain and body, and providing treatment focused on stabilization, emotional safety, and nervous-system regulation.
A: Trauma-focused psychiatry considers triggers, hyperarousal, dissociation, avoidance patterns, and the impact of trauma on relationships and functioning. Treatment plans prioritize gentleness, pacing, collaboration, and patient choice.
Q: What medications are helpful for trauma-related symptoms?
A: Medications may target anxiety, depression, nightmares, sleep disruption, emotional reactivity, and hyperarousal. Your provider designs a plan that supports stabilization without overwhelming your system.
A: Yes. Collaboration between your psychiatrist and therapist helps ensure consistency across medication management, grounding skills, and trauma processing.
A: Yes. Trauma can affect people long after the event. Trauma-focused psychiatric care helps reduce symptoms, build resilience, and support healing at any stage.
